Steven Holzman, MD - Gynecomastia Specialist


Dr Holzman did an excellent job with my recent surgery and follow up! His professional skills are superb and his bedside manner is both caring and reassuring. A good listener, Dr Holzman took the time with me to make sure he understood my needs and expectations. His office staff is professional and personable! They were great to work with!
Your Guide to Gynecomastia
- Meet Dr. Holzman
- What is Gynecomastia?
- Gynecomastia Symptoms
- Gynecomastia Grades
- Gynecomastia Causes
- Gynecomastia During Puberty
- Gynecomastia vs. Pseudogynecomastia
- Gynecomastia Diagnosis
- What is Male Breast Reduction?
- Gynecomastia Procedure
- Gynecomastia Surgery Recovery
- Gynecomastia Surgery Recovery Timeline & Tips
- General Recovery Tips
- Gynecomastia Surgery Scars
- Non-Surgical Gynecomastia Treatment
- Gynecomastia Surgery Cost
- Additional Gynecomastia FAQs
What is Gynecomastia?
Gynecomastia is a condition characterized by the development of excess glandular and/or fatty tissue in the chest region of some males. This excess tissue can be a frustrating and emotionally taxing reality for many men to deal with, as it often creates the appearance of having breasts. Fortunately, experienced plastic surgeon Steven Holzman, MD, can help treat gynecomastia and restore a flatter, smoother, more masculine chest appearance.
What Are the Symptoms of Gynecomastia?
While gynecomastia is generally considered a medically benign condition, it can still lead to a variety of uncomfortable symptoms, including:
- Swollen, tender breast tissue
- Nipple sensitivity and/or chafing
- Asymmetrical chest development
- A conical or “pointed” chest appearance
- Fat accumulation and skin sagging around the chest
- Nipple discharge
- Embarrassment when wearing fitted clothes or going shirtless
- Lower self-esteem
Dr. Holzman believes that every man deserves to feel comfortable and confident. He tailors male breast reduction surgery to help those afflicted with gynecomastia restore a flatter, more masculine chest appearance for improved confidence and quality of life.
Grades of Gynecomastia
Gynecomastia is generally classified across four different grades of severity. When the condition is not corrected, it will typically worsen over time, with the glandular tissue development leading to increasingly prominent aesthetic disruption.
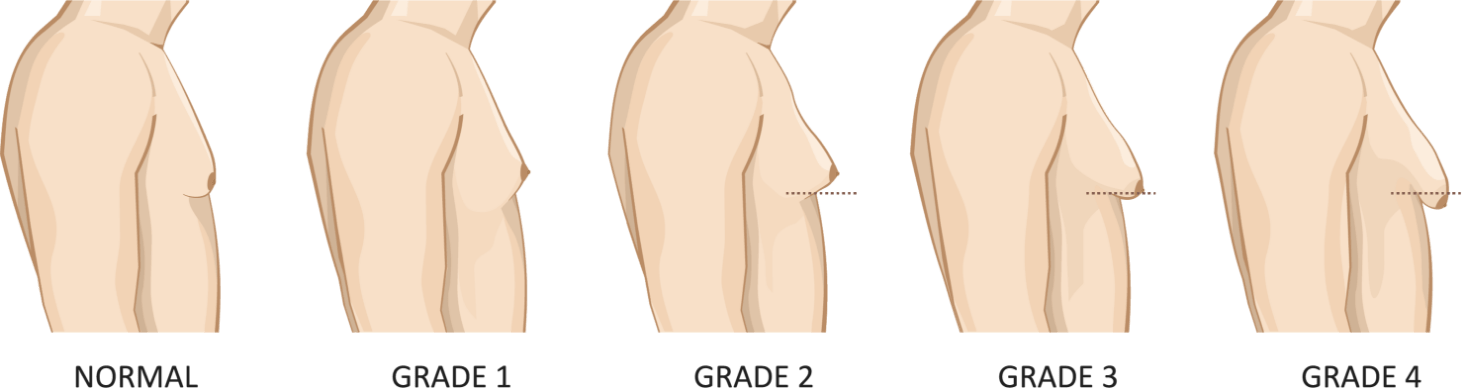
Grade 1
The early stages of gynecomastia are characterized by tissue growth centered around the nipples and areolas, often producing a pointed or conical shape. This new tissue is often also puffy and discolored. Treatment is generally simplest and most effective at this stage of gynecomastia.
Grade 2
Grade 2 gynecomastia sees the new tissue growth from grade 1 expanding beyond the nipple-areola region and causing the broader chest region to fill out. The texture of the chest may also begin to change, with the underlying glandular tissues feeling firm and tight, while the fatty outer tissues feel soft and pliant.
Grade 3
Grade 3 gynecomastia is typically characterized by increased skin laxity and significant tissue expansion. As the skin begins to sag—typically along the inframammary fold—the chest takes on a drooped appearance. Patients often find that their gynecomastia is significantly more aesthetically disruptive at Grade 3, becoming visible even through clothing. Treatment at this phase may also incorporate skin excision and/or nipple repositioning, depending on the age of the patient and the condition of the skin.
Grade 4
Grade 4 is the most advanced stage of gynecomastia, and it is characterized by severe skin laxity and breast ptosis, or drooping. Most cases typically require both glandular excision and liposuction to achieve optimal results. Some men may also choose to undergo an additional procedure such as a free nipple graft, which is designed to return the nipple-areola complex to a more ideal position on the chest.
What Causes Gynecomastia?
The appearance of enlarged male breasts can be brought on by a number of factors, including:
- Natural hormonal fluctuations, such as those experienced during puberty
- Low testosterone levels, which are often seen in men ages 50 and older
- Specific medications, including certain steroids, androgen inhibitors, cancer treatments, heart medications, antidepressants, and antibiotics
- Alcohol and drug usage, including frequent use of marijuana
- Health conditions such as kidney and liver failure, hyperthyroidism, hormonally active tumors, and general malnutrition
- Major weight fluctuations, which can cause fat cells to gather in the chest (this type of breast enlargement is actually known as “pseudogynecomastia”)
- Most gynecomastia is actually idiopathic which means that there is no known causative factor—it just develops in some males
Gynecomastia During Puberty
Symptoms of gynecomastia can develop during puberty as the body experiences rapid hormonal changes. Puberty-induced gynecomastia is fairly common in boys between the ages of 12 and 16, with an estimated 50% of the male population experiencing some degree of breast growth during their teenage years. In many cases, gynecomastia that develops during puberty resolves on its own as the hormonal fluctuations subside. However, for patients whose male breast growth persists into adulthood, surgical intervention may be the most effective solution.
Gynecomastia vs. Pseudogynecomastia
Although both conditions are often referred to as gynecomastia, there are actually two general types of male breast enlargement. True gynecomastia refers to cases where expanding glandular tissues are causing abnormal chest enlargement. This condition is typically brought about by an imbalance between testosterone and estrogen. When testosterone levels drop below estrogen levels, estrogen can encourage glandular breast tissue development, leading to male breast growth. Hormonal fluctuations occur naturally during infancy, puberty, and in men over the age of 50, but low testosterone levels can also be triggered by certain medications, lifestyle habits, and health concerns. In many cases, gynecomastia brought on by puberty will fade on its own once the body is able to regulate its hormone levels. However, when the condition presents in adult males or does not improve in adolescents after two years, surgery is oftentimes the most comprehensive and effective solution.
Pseudogynecomastia refers to male breast growth that occurs as a result of excess fatty tissue. Major weight fluctuations can lead to an accumulation of fat cells in the chest region, often causing the area to grow and/or swell. As the fat cells accumulate, the skin may also begin to expand and, in some cases, droop, resulting in the appearance of male breasts. In some cases, patients may have an excess of both glandular and fatty tissues. During your consultation, Dr. Holzman can help you determine the cause of your enlarged male breasts and make treatment recommendations accordingly.
How is Gynecomastia Diagnosed?
Clinically, gynecomastia is diagnosed after your doctor or surgeon conducts a comprehensive physical examination and reviews your medical history. An important part of this process is to determine whether you are experiencing true gynecomastia, pseudogynecomastia, or a potentially malignant issue, such as breast cancer.
One of the primary methods of screening for true gynecomastia versus pseudogynecomastia is the “pinch test.” Upon manual exam, Dr. Holzman can use his thumb and forefinger to assess the deep breast tissue located below the nipple. If the patient has true gynecomastia, a firm, rubbery mass can typically be felt, indicative of glandular tissue development. If the patient has pseudogynecomastia, the tissue will feel soft and fatty. Depending on your symptoms, medical history, and the results of your physical examination, your doctor may also order other diagnostic tests, such as blood work or a mammogram.
What is Male Breast Reduction?
Male breast reduction refers to a surgical procedure that is designed to help remove the excess skin and tissues that contribute to the appearance of enlarged male breasts. Dr. Holzman has been treating gynecomastia for years, and he offers multiple different techniques that are designed to meet the unique needs of each patient. Treatment options include:
- Liposuction is often employed in cases where the appearance of male breasts is primarily caused by an abundance of fatty tissue, also known as pseudogynecomastia.
- Glandular breast tissue surgery is designed to remove excess glandular tissues, which contribute to the pointed appearance of the nipple-areola complex and increased chest fullness.
- In most cases, both liposuction and glandular tissue removal may be necessary to achieve the desired results. This typically occurs in cases where there is an abundance of both types of tissue.
- Body contouring is often incorporated into gynecomastia treatments in order to remove any excess skin and sculpt the remaining tissues for an optimal chest aesthetic.
How is the Male Breast Reduction Procedure Performed?
During your consultation, Dr. Holzman will evaluate your specific needs and aesthetic goals in order to determine the optimal approach to treatment. For men whose gynecomastia is primarily caused by excess fatty tissues, liposuction can be employed in order to gently and effectively reduce breast volume. In cases where excess chest volume is being caused by glandular tissue, Dr. Holzman will create a small incision around the nipple and remove an appropriate amount of tissue. For men who have an excess of both fatty and glandular tissues, these two techniques can often be combined in order to yield the most comprehensive results.
Liposuction
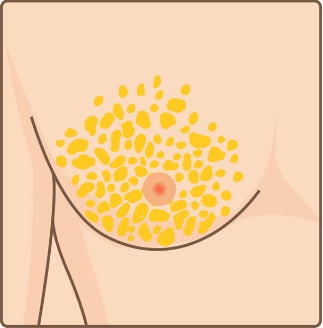 Excess fat tissue
Excess fat tissue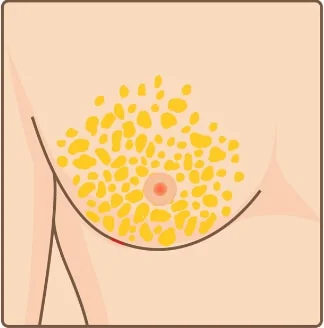 Incision
Incision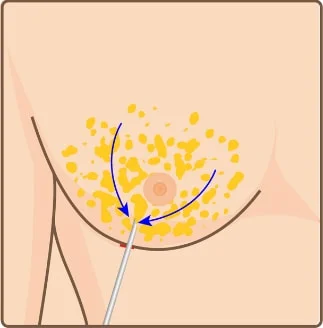 Liposuction removes breast fat
Liposuction removes breast fat Suture
Suture
Glandular Breast Tissue Surgery
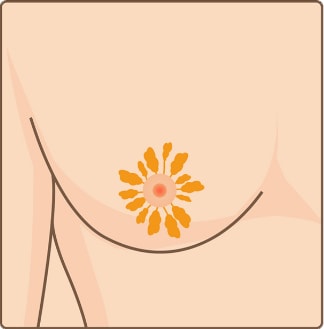 Excess mammary gland tissue
Excess mammary gland tissue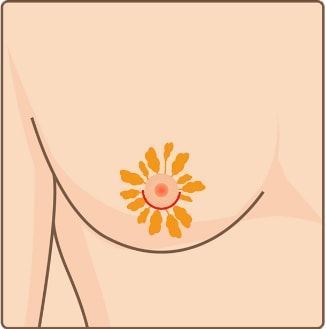 Incision
Incision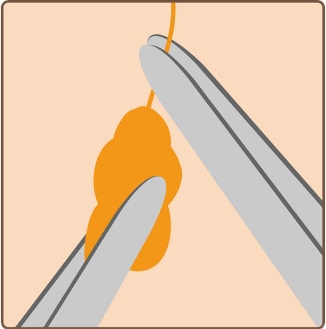 Remove excess mammary gland tissue
Remove excess mammary gland tissue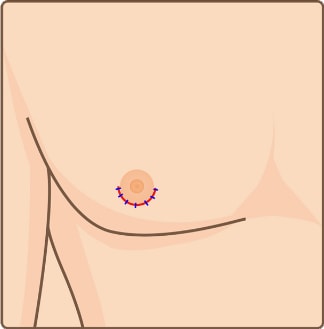 Suture
Suture
What Can I Expect During Gynecomastia Surgery Recovery?
The precise details of recovery will vary based on a number of factors, including the treatment method utilized, the amount of tissue that was removed, and your natural rate of healing. That said, patients should expect to avoid strenuous activity for at least the first few weeks following surgery, and they should carefully follow all of Dr. Holzman’s postoperative care instructions. After your procedure, Dr. Holzman will provide you with a compression garment that is designed to hold a set of foam pieces in place over the surgical site. This compression garment should be worn for approximately 18 hours a day for four weeks to aid healing and prevent bruising.
Following surgery, you may be prescribed narcotic pain medication to help aid sleep and recovery. Driving and the operation of heavy machinery should be avoided while you are taking these medications. Some patients even find that their post-surgery discomfort can be managed almost entirely with over-the-counter medications. Moderate swelling and bruising are common occurrences after surgery, and patients may utilize a cold compress or ice pack if they choose. Itching along the suture lines may also occur, but Dr. Holzman advises patients to avoid scratching, as this can disturb the surgical site. Instead, you may take a Benadryl® or other over-the-counter anti-itching medication. If you experience heightened nipple sensitivity, a gentle one to two minute massage a few times a day may help soothe the area.
Gynecomastia Surgery Recovery Timeline & Tips
Recovery Timeline
- What’s Happening: Swelling, bruising, and mild-to-moderate discomfort.
- Care Tips:
- Rest and minimize unnecessary movement (aside from short, periodic walks to promote circulation)
- Wear the compression garment consistently.
- Take prescribed medications as directed.
- What’s Happening: Swelling begins to reduce; mild tightness and itchiness may persist.
- Care Tips:
- Continue light walking to promote circulation but avoid anything more strenuous.
- Keep the incision area clean and dry, and avoid scratching.
- Attend any scheduled follow-up appointments with your surgeon.
- What’s Happening: Bruising fades; you’ll feel more comfortable.
- Care Tips:
- Continue wearing the compression garment.
- Gradually increase light activities, avoiding heavy lifting or chest-focused movements.
- Monitor the incision area for signs of infection, like redness or unusual discharge.
- What’s Happening: Swelling significantly decreases, and most discomfort resolves.
- Care Tips:
- Return to light exercise, such as walking or gentle cardio.
- Avoid heavy lifting or strenuous chest workouts.
- Check in with your surgeon for a progress evaluation.
- What’s Happening: Residual swelling subsides; scars begin to fade.
- Care Tips:
- Resume all normal activities, including exercise (once cleared by your surgeon).
- Protect scars from direct sunlight to ensure proper healing.
- Watch for final results as your body settles into its new contour, which may take several months.
General Recovery Tips
- Wear Your Compression Garment: Critical for the first four to six weeks to reduce swelling and support healing.
- Stay Hydrated and Eat Well: A balanced diet that is high in protein supports tissue repair.
- Avoid Smoking and Alcohol: These can slow down the healing process.
- Be Patient: Full results may take several months to appear.
Will I Have Scars After Gynecomastia Surgery?
As is the case with all surgical interventions, gynecomastia patients will have some minor scarring around the incision site(s) after the procedure. However, Dr. Holzman has years of experience performing male breast reduction surgery, and he can position the incision lines so that they will blend in as naturally as possible with the surrounding tissues. The precise size and location of the incisions will vary depending on the severity of the condition being treated and the treatment method utilized.
- For patients who undergo liposuction, a small incision will be placed at the edge of the areola and occasionally along the inframammary fold—the crease where the chest meets the rest of the abdomen. Once the incisions have properly healed, they typically blend in with the natural contour of the chest.
- For patients receiving a glandular tissue reduction treatment, the incision is usually made around the outer edge of the areola. Once healed, most patients find that their scars blend in quite well with the surrounding tissues.
While the majority of patients find that their gynecomastia treatment scars do not present a significant aesthetic disruption, Dr. Holzman does offer a variety of options for those who require scar treatment. In some cases, medical-grade skin care products can help reduce the appearance of scars or protect them from sun damage. Rarely, a scar-revision procedure may be necessary to help them blend in better with the surrounding tissues. Generally most patients find their scars fade and disappear rapidly and become undetectable.
Is It Possible to Treat Gynecomastia Without Surgery?
Most patients with true gynecomastia cannot achieve their desired male breast reduction results without surgery. Since true gynecomastia is caused by excess glandular tissues, non-surgical interventions such as weight loss and exercise are unlikely to have a significant impact. Indeed, some men even find that certain pectoral exercises actually cause their gynecomastia to become more prominent, as the developing muscles push the expanded glandular tissues further out from the chest wall. In order to effectively target and reduce the amount of excess glandular tissue, male breast reduction surgery is often the only reliable solution.
That said, men experiencing pseudogynecomastia, which is caused by excess fatty tissues, may see some improvement in their condition by losing weight or strengthening their pectoral muscles. Unlike glandular tissues, fatty tissues are sometimes responsive to non-surgical efforts. However, many men experiencing pseudogynecomastia are still unable to achieve their desired chest appearance through diet and exercise alone. Liposuction, which is designed to target specific pockets of unwanted fat, can help improve the chest contour and restore a flatter, smoother appearance.
How Much Does Gynecomastia Surgery Cost?
The precise cost of male breast reduction will vary based on several factors, including the severity of the gynecomastia and the treatment method utilized. That said, the typical cost for a male breast reduction procedure at our Austin and Round Rock, TX practice averages around $10,000. This price includes the facility costs, anesthesia, and surgeon’s fee. During your consultation, Dr. Holzman and our experienced staff will provide you with a more precise price quote based on your unique needs. If you have additional questions about the potential costs associated with gynecomastia surgery, we encourage you to contact us directly.
“Dr. Holzman and his staff are an incredible group of people. They go out of their way to support their patients, and allow them to be well-informed and comfortable with the procedures they’re looking for. I am so glad to have had Dr. Holzman as my surgeon.”
Our Patient Results
Additional Male Breast Reduction Frequently Asked Questions
-
Does gynecomastia hurt?
In the majority of cases, gynecomastia is not a physically painful condition. However, some men do experience tenderness, swelling, and/or itchiness of the breast tissue and nipples. The emotional discomfort associated with male breast development can also take a serious toll on a man’s self-confidence and mental health and once repaired, the minimal pain associated with the procedure is far outweighed by the benefit of renewed confidence and appearance at the pool and in front of the mirror. -
Does gynecomastia go away on its own?
Whether or not gynecomastia can resolve on its own depends on what is causing the condition. When breast development presents in adolescents as a result of hormonal changes during puberty, it often does go away naturally as the levels of estrogen and testosterone in the body level out. Those experiencing pseudogynecomastia may also be able to achieve a flatter, firmer chest appearance by losing weight and doing pectoral exercises. However, true gynecomastia in adults typically does not resolve without intervention, and it is important to consult with a medical professional to determine causality. From there, a personalized treatment plan can be developed to help halt further breast development and restore a more masculine chest appearance. -
Can gynecomastia be prevented?
There are a number of different factors that can contribute to the development of gynecomastia, and not all of them can be prevented or controlled. That said, there are things that patients can do to minimize the risk of developing the condition. Maintaining a healthy diet and stable body weight can prevent the accumulation of fatty tissue in the chest, mitigating the chance of developing pseudogynecomastia. It can also be beneficial to avoid substances known to increase one’s risk of male breast growth, including marijuana, alcohol, anabolic steroids, and other substances often obtained at the gym or unauthorized websites offering muscle build up and such. -
What are some tips for the first 24 hours after gynecomastia surgery?
In the 24 hours following male breast reduction surgery, Dr. Holzman recommends taking your prescribed medications at regular intervals. You may begin eating solid foods as you are able to tolerate them. To help reduce nausea, drink a lot of fluids and eat primarily simple foods that are easy to digest, such as saltine crackers or plain rice.
You should also be sure to wear your compression garment continuously. It should remain clean, dry, and properly adjusted 24 hours a day for the first few days after gynecomastia surgery. Be sure to replace any gauze that has been saturated, and avoid strenuous activities of all kinds.
-
How should I sleep after gynecomastia surgery?
For the first week after male breast reduction surgery, you should sleep on your back and maintain a slight elevation to promote blood flow and healing. -
What should I eat after gynecomastia surgery?
After surgery, we suggest starting with soft, high-protein foods that are easier to eat, like yogurt, soup, and protein shakes, before working up to more solid foods. Dr. Holzman recommends avoiding foods that are high in sugar or salt, as these can contribute to inflammation and swelling. It’s important to remain hydrated throughout your recovery process and continue to drink plenty of clear fluids. Over the long-term, eating a nutritious diet and maintaining an active lifestyle can help safeguard your chest contouring results as well as your overall health. -
Can I bathe after gynecomastia surgery?
Generally, patients should avoid bathing after male breast reduction until cleared by their surgeon. It is difficult to get in and out of the bath without putting your recent surgery at risk for bleeding. You can use a hand held shower head to rinse the lower half of your body but your chest must stay dry. -
Can I shower after male breast reduction surgery?
You may resume showering following your first postoperative visit with Dr. Holzman, which is typically scheduled for a few days after your male breast reduction procedure. In order to protect your incision site, remove your compression garment before showering and gently pat the surgical site dry before replacing the garment. If you notice any drainage from the incision sites, you may place a gauze pad or liner on the inside of the compression garment to keep it dry and clean. -
Is it normal for one breast to heal more quickly than the other after gynecomastia surgery?
It is completely normal for the different sides of the chest to heal at different rates following male breast reduction. You may notice that one breast has more swelling or is more sensitive than the other. In some cases, they may even appear to be different shapes or sizes. However, as your chest heals, you should notice the chest settling into a more natural, even appearance. -
Why does the skin over my chest look shiny after gynecomastia surgery?
The skin around the surgical area may appear shiny for the first few weeks after your male breast reduction surgery. This is typically caused by swelling, and it should subside with time. -
What can I do to help reduce scarring after gynecomastia surgery?
New scars will always appear fairly prominent, oftentimes in varying shades of red, pink, and purple. In order to reduce the appearance of your male breast reduction surgery scars, you should avoid sun exposure and ensure that you always apply sunscreen when your chest will be exposed. Dr. Holzman can also recommend medical-grade scar reduction treatments and products to help further minimize the aesthetic impacts. Generally speaking, scars on the chest may take a year or more to fully heal, but generally look great after three months. The final appearance of the chest takes three to six months to fully achieve but once again, you will be presentable without a shirt after about two weeks, depending on the amount of bruising you have. -
What can I expect during my first post-op visit after gynecomastia surgery?
Dr. Holzman usually schedules your first postoperative visit on the fourth or fifth day following male breast reduction surgery. During this appointment, he will carefully remove the dressings from the surgical site and check your incisions to ensure that they are set and healing properly. He will then remove the foam pieces from your compression garment. After evaluating your incision-sites and discussing your progress with you, he can provide more detailed instructions that are designed to fit your individual lifestyle and needs. -
When will my sutures be removed after male breast reduction surgery?
The sutures that Dr. Holzman uses during gynecomastia surgery are absorbable and will not need to be removed. Patients do not need to disturb their dressings unless they become wet or are saturated by discharge from the surgical site, in which case the gauze should be replaced. Steri-strips will be placed over the incisions after surgery, and these should remain in place until you are otherwise directed. -
Will insurance cover male breast reduction?
In most cases, gynecomastia surgery is considered an elective procedure. As such, it is unlikely to be eligible for insurance coverage. That said, we encourage you to reach out to our office to discuss financing and payment plan options. We are committed to ensuring that high-quality aesthetic treatment is available to patients on virtually any budget. -
Are there age requirements for gynecomastia surgery?
While there are no specific age limitations for gynecomastia surgery, it is generally recommended that patients be over the age of eighteen and in good overall health. In many cases, adolescent gynecomastia resolves on its own once the hormonal fluctuations associated with puberty subside, rendering surgery unnecessary. Dr. Holzman takes the time to consult with each patient in order to determine the most appropriate course of action for their unique case.
Some patients also wonder whether there is a point at which they may be “too old” for gynecomastia surgery. Ultimately, there is also no upper age limit for male breast reduction. However, certain age-related health concerns can make undergoing any type of surgery more risky, so it is important to discuss your medical history with a qualified professional before pursuing treatment.
-
Is it possible for excess male breast tissue to return after gynecomastia surgery?
Gynecomastia surgery permanently removes excess glandular and/or fatty tissue that may cause the appearance of male breast development. That said, gynecomastia has a variety of different underlying causes, and it can redevelop in some cases. For instance, significant weight gain can cause pseudogynecomastia to develop (or redevelop), and certain medications (such as steroids) can sometimes promote further glandular tissue growth. During the consultation and recovery process, your surgeon can provide advice on how to limit the likelihood of gynecomastia returning so that you can continue to enjoy your aesthetic results over the long-term. -
Will I lose nipple sensation after male breast reduction?
In the immediate aftermath of gynecomastia surgery, many men experience a temporary numbness or reduction in nipple sensation. However, in the majority of cases, nipple sensitivity should return over the course of the next few weeks to months. -
Can exercise get rid of gynecomastia?
True gynecomastia (which is caused by glandular tissue development) cannot typically be treated with exercise. Indeed, pectoral exercises can sometimes make the aesthetic impacts of true gynecomastia more prominent by pushing the excess tissue outward. That said, patients with pseudogynecomastia (which is caused by excess fatty tissue) may see some improvement in their condition with diet and exercise. However, male breast reduction surgery is typically the only way to address both excess tissue and skin for comprehensive results. -
Can physician-supported weight management shrink enlarged male breasts?
Physician-supported weight management can help reduce excess fat in the chest, which may improve the appearance of enlarged male breasts when the issue is primarily related to weight. However, true gynecomastia involves excess glandular tissue, which does not shrink with weight loss alone. While medical weight management can enhance overall contour and support healthier results, surgical treatment is often required to fully address glandular enlargement. A consultation with Dr. Holzman can help determine the most effective approach for your specific needs. -
When should I consider gynecomastia surgery after weight loss?
You may consider gynecomastia surgery once you’ve reached a stable, healthy weight and maintained it for several months. Significant weight loss can reduce excess chest fat, but if firm and enlarged glandular tissue remains, surgery may be the most effective way to achieve a flatter, more contoured chest. In most cases, it’s also best to wait until your weight has plateaued to ensure your final results are long-lasting. If loose skin or persistent fullness continues despite your efforts, Dr. Holzman can help determine whether you’re ready for surgery and which approach can best address your concerns.






